Insomnia. Most people have experienced insomnia at one point or another. Sometimes, we may experience insomnia for a few days or longer. Although the symptoms might seem quite simple,insomnia is a complex condition with a wide variety of causes.
Insomnia is a very common condition. Thirty-four percent to forty percent of Americans have experienced insomnia symptoms in the last year. Ten to fifteen percent are suffering from chronic insomnia.
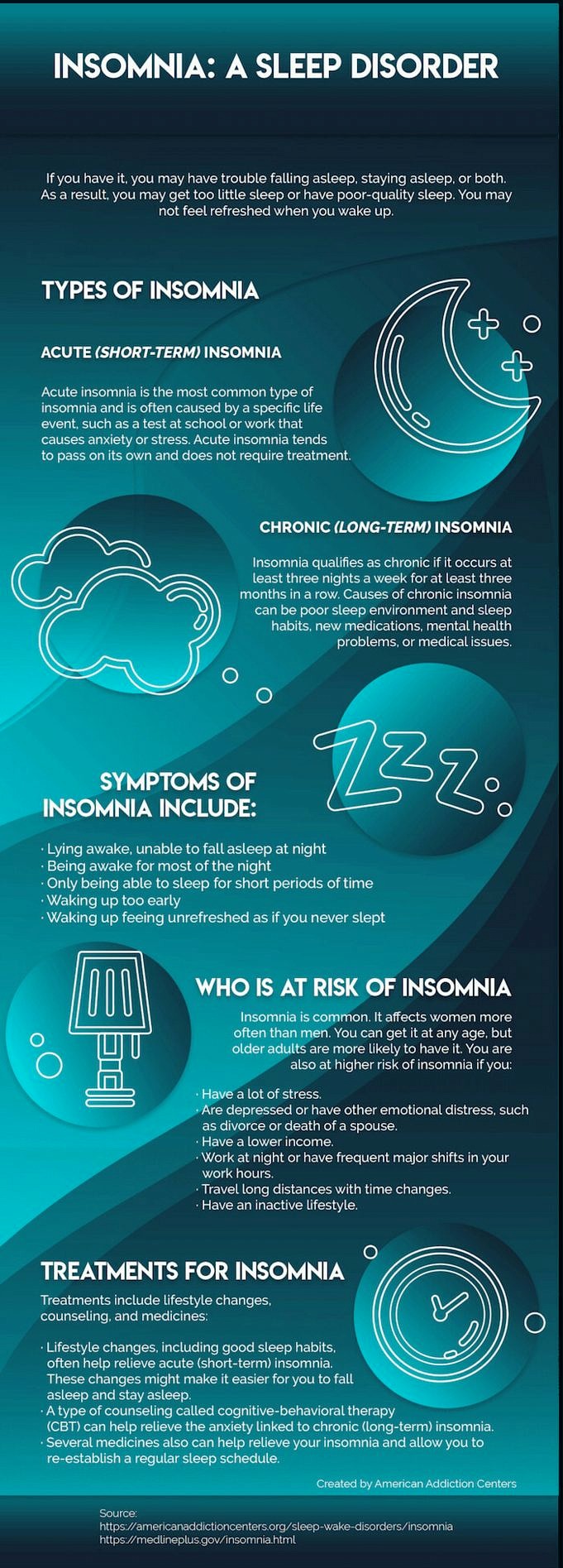
Insomnia, also known as sleep disorder, is defined as inability to fall asleep or stay asleep.It could be transient, acute, or chronic. It may be transient, acute, or chronic. Insomnia is by far the most common sleep disorder, affecting as much as half the worlds population at some point in their lives.
Insomnia is characterized by its interference with daytime functioning.. This difficulty may take the form of fatigue, trouble concentrating, irritability, or memory lapses. Along with impulsiveness and depression, microsleep episodes can occur.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldnt taken as medical advice, and it shouldnt take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Insomnia Symptoms
Insomnia is characterized by the inability to fall asleep, stay asleep or go back to sleep.Many insomniacs suffer from a variety of cognitive and physical effects. However, they are not the primary symptoms and can be shared with those who suffer from sleep deprivation or other sleep disorders. Insomnia can, however, produce a wide range of effects, including:
- Feeling tired/groggy when you wake up
- Daytime fatigue
- Depression or anxiety
- Irritability or mood swings
- Concentration is difficult
- Trouble retaining new information
- Reduction in coordination
- An increase in errors and accidents on the job or at home
- Performance at work has been reduced
- Trouble engaging in social activities
In addition, insomnia sufferers may experience impaired decision-making , relationship difficulties, and reduced quality of life. They may use sleeping pills or other supplements to help them fall asleep or stay asleep.Sleep-related anxiety that begins with a transient bout of insomnia may become a persistent issue.
The symptoms of insomnia can vary from mild to severe and can fluctuate over time. Sometimes symptoms can improve at different times in life, and then recur.
Insomnia Fact: A person who sleeps less than the average seven to nine hours each night but does not suffer from symptoms of insomnia may be whats called a short sleeper. Short sleepers feel refreshed on less sleep than is usual for most of us, often five hours or fewer
Insomnia Vs. Sleep Deprivation- Whats The Difference?
They can be confused because insomnia and sleep deprivation have some cognitive and physical effects. Both can cause fatigue and trouble concentrating but they are not the exact same.A person who is willing to sleep without any support or assistance. Insomnia refers to the inability to fall asleep, stay asleep, or return to sleep..
One can experience sleep deprivation when studying, traveling, or caring for a sick child.The person who is sleeping-deprived can sleep if given the chance. However, a person with insomnia can’t sleep, even if they are allowed to..Insomnia concerns sleepQuality, while sleep deprivation concerns sleepquantity.
While insomnia and sleep deprivation might have important differences, the symptoms are not the same. Not exactly. Sleep deprivation can result in daytime sleepiness, poor concentration, memory problems, and decreased emotional control.Some studies show similar deficits in people suffering from insomnia, but there are some significant distinctions.
Hyperarousal of the sympathetic nervous system may be at play in some cases of chronic insomnia, preventing sleep and a feeling of sleepiness at night. This hyperarousal may also prevent insomnia sufferers from experiencing the same daytime sleepiness and cognitive impairments experienced by those who are sleep-deprived, even when they operate on the same amount of sleep.
This could mean that current testing techniques dont adequately show the physical and cognitive effects of chronic insomnia, or it could mean that, though insomniacs are similarly affected by lack of sleep, hyperarousal of their nervous systems overrides these impairments, allowing them to feel more alert.
The ability of insomnia sufferers to fall asleep quickly is another difference.. Even when deprived of their usual amount of sleep, chronic insomniacs tend to fall asleep less quickly than the sleep-deprived, wake up sooner, and have more trouble staying asleep.
Insomnia Symptoms And Their Causes
Insomnia used to be divided into two categories- primary and secondary. Primary was thought to be insomnia without an apparent cause, while secondary was thought to be caused by something else, such as another medical condition, mood disorder, or medication. Recent research has shown that almost all cases of insomnia can be attributed to one of these categories.
While insomnia symptoms are more common than insomnia disorder, they are less common.. Insomnia symptoms are experienced by many of us periodically throughout life, and may be the result of:
- Stress
- Depression and mood disorders
- Trauma or grief
- Illness
- Chronic pain
- Sleep disorders like sleep apnea and restless leg syndrome are known as sleep disorders.
- Medications, especially those with a stimulant effect, such as ADHD treatments and decongestants
- Alcohol
- Jet lag and daylight saving time
Although symptoms of insomnia can be temporary, they are often self-explanatory.When a stressor is gone, an illness can be treated or the normal sleep schedule resumed. Although treatment is not usually necessary, anxiety and other negative symptoms can persist. This may lead to wakefulness at night or the development of insomnia disorder.
Insomnia Disorder And Its Causes
Insomnia disorder goes beyond the symptoms of insomnia. Commonly known as chronic insomnia, insomnia disorder occurs at least three nights each week for three months or longer. About 10% of Americans suffer from insomnia disorder.
Contradictory as it may seem,Sleeping time is not the only factor that causes insomnia.. Insomnia disorder concerns the inability to fall asleep, stay asleep, or fall back to sleep.
Insomnia disorder typically results from a negative conditioned response to bedtime, the attempt to sleep, or the sleeping environment. Less commonly, it may be caused by neurological difficulties such as head injuries.
A negative conditioned response to sleep may cause hyperarousal of the bodys sympathetic nervous system. This can lead to an increase in heart rate, cortisol secretion and metabolic rate during sleep and wake hours. Studies of identical twins support the hypothesis that hyperarousal of the bodys systems may contribute to chronic insomnia.
Additionally,There may be fundamental differences between insomniacs and those who sleep well.. These variations could also be a sign of hyperarousal in chronic insomnia sufferers.
Although symptoms of insomnia can be caused by many factors, such as stress at work or alcohol consumption, they are generally not the root cause.Insomnia is a chronic disorder that can be difficult to treat..
Causes Of Insomnia Symptoms In Women
For women, hormonal changes, menopause, and pregnancy may contribute to the inability to sleep. As they age, women are more likely to experience insomnia symptoms. Studies that show sleep patterns changing between girls and boys starting in puberty support this theory.
Women suffer in greater numbers than men from medical conditions that may cause symptoms of insomnia, including certain autoimmune diseases, migraines, and pelvic pain. They are at greater risk for osteoporosis which can lead to joint and spine pain, and make it difficult to sleep.
Women are also more likely to have to care for elderly relatives and be single parents. These stressors may contribute to higher rates of insomnia symptoms, as well as fewer hours available to sleep.
How Can Insomnia Be Diagnosed?
A simple self-reporting by the patient of their symptoms can often diagnose insomnia.Because people undergoing sleep studies often sleep less than they would in their usual environment, such studies are rarely helpful for diagnosing insomnia disorder.
A doctor may also need to know about your symptoms.
- Ask about your sleeping habits and social environment
- Suggest you keep a sleep diary to track your sleep patterns and identify factors that might contribute to your insomnia issues
- To better understand your sleeping habits, ask that you complete one or more insomnia tests. These might include questionnaires such as the Insomnia Severity Indexor a mental health examination
Insomnia Fact: Human beings are the only mammals known to willingly delay sleep
Insomnia: Three Subtypes, Three Stages
A diagnosis of insomnia may be further broken down into more detailed sub-types and stages.The duration of the condition is what distinguishes the three main types of insomnia.. Although the symptoms may be similar, treatment and prognosis can vary depending on final diagnosis.
The Three Main Sub-Types Of Insomnia
1.Transient insomnia symptoms. It can last from a few days up to several months and it can be intermittent or continuous.Anxiety that can accompany temporary insomnia symptoms can lead to chronic insomnia.These symptoms may be caused by: Causes of these symptoms may include:
- An emotionally stressful event, such as a death, new job, move, or birth of a baby
- Poor sleep hygiene is a major cause of insomnia. Noise, bright light, late meals, use of electronics, alcohol, and caffeine are common contributors to transient insomnia
- Circadian rhythm disturbances, such as jetlag or a change in work schedule, can cause disruptions.
- You may need to adjust to a new environment such as a hotel, new bed or unfamiliar house.
- Adjustment to a higher altitude
2.Acute Insomnia Symptoms.
Sleeplessness that persists up to three months. Like transient insomnia, acute insomnia may come and go. Common triggers include:
- Emotional conflict or difficulty
- Shift work
- A death or traumatic event
- Pain or illness, such as sleep apnea, asthma, acid-reflux disease, or diabetes
- Stressful life events such as a move or divorce can cause disruptions in your life.
3.Chronic Insomnia, or Insomnia Disorder. Persistent insomnia symptoms for more than three months. Although there are many causes for insomnia symptoms, most people only have one cause of insomnia disorder. Insomnia disorder is usually caused by:
- A conditioned response to bedtime, the attempt to sleep, or the sleeping environment. Hyperarousal of the sympathetic nervous system may be part of this response. This type of conditioning is responsible for the majority of insomnia disorders.
- Head injuries and other medical conditions. These cause a proportionally small number of insomnia disorder cases
The Three Stages Of Insomnia
The experience of insomnia may be different according to the time of night during which it occurs. It can happen at night’s beginning, in the middle of the night or in the early morning. The trigger may be different depending on the time it occurs. An insomnia sufferer may go through one or all of these stages, which may happen every night, or come and go. The three stages include:
1.Onset Insomnia. Insomnia is the inability or inability to fall asleep for longer than 30 minutes after getting up. This type of insomnia is often associated with a conditioned negative response to bed, as well as elevated levels of anxiety and hyperarousal of the nervous system.
2.Also known as Sleep Maintenance Insomnia or Middle Insomnia. This type of insomnia can be described as waking up during the night and spending extended periods awake. This type of insomnia could be caused by illness, another sleep disorder such as nightmare disorders, chronic pain, or other causes.
Consuming alcohol is another common cause of insomnia in the middle. Although alcohol can make it easier to fall asleep, it can also cause you to wake up during the night after the central nervous system effects wear off.
3.LateInsomnia. Late insomnia is characterized by waking up too early in the morning. This can happen as the sleep patterns of older people change. This is also common in mood disorders such as depression. Anxiety and stress can cause an internal alarm system that causes a consistent, early-morning awakening.
Treatments for insomnia can be tailored to the specific sub-type or stage of a patient’s sleep disorder.. For instance, those experiencing grief may have transient insomnia symptoms and wake early in the mornings, while those with chronic pain may lie awake or be unable to fall back to sleep during the night. Some sufferers may find psychotherapy helpful, while others might benefit from cognitive behavior therapy and a reduction in time spent in bed.
What Can Narcolepsy Do To Insomnia?
One of the most well-known forms of hypersomnia is Narcolepsy. This is a condition that causes sleep problems such as excessive sleepiness at night and unusual sleepiness during the day. Narcolepsy appears to be an autoimmune disease triggered by a viral illness, usually in childhood or adolescence.
Symptoms of narcolepsy include sleeping up to sixteen hours each day or more, needing to take naps after a full nights sleep, grogginess, suddenly muscle weakness while laughing or experiencing strong emotion, andinsomnia?
It may seem impossible for insomnia symptoms and narcolepsy to co-exist, but often they do. Narcolepsy can cause excessive daytime sleepiness as well as interrupted sleep cycles and sleep disruptions. Sleep is typically not restorative, and may be disturbed by parasomnias such as sleep paralysis and hallucinations.
People with Narcolepsy may experience overwhelming exhaustion during their day but not be able to fall asleep at night or wake up feeling exhausted.. This is often due to disrupted nighttime sleeping, or DNS.
DNS is different from traditional insomnia in that patients with narcolepsy don’t usually have trouble falling asleep. However, they often experience disturbed sleep and middle insomnia along with other symptoms typical of narcolepsy. DNS can be part of the constellation of symptoms associated with narcolepsy, leading to periods of poor sleep despite the amount of time sufferers must spend in bed.
Insomnia And Its Health Consequences
Although occasional insomnia symptoms can be hard to avoid,insomnia that lasts more than a few weeks or becomes chronic may have serious health effects.
Insomnia may lead to long-term sleep debt, which can result in disruptions to metabolism, mood, and glucose tolerance.
These are some of the possible health effects of insomnia:
- Impaired immune function
- Increased risk of chronic disease including diabetes, heart disease, and hypertension
- Increasing risk of mood disorders like anxiety and depression
- Difficulty concentrating
- Retention of new information is difficult
- Impairment in judgment, reasoning, or problem-solving ability
- Impaired performance at work or school
- Increased risk of errors and accidents, due partly to impaired reaction times
- Diminished sex drive and fertility
- Increased signs of aging, particularly in the skin
- Higher risk of weight gain
- Life expectancy has fallen
Although chronic insomnia sufferers may experience hyperarousal of their central nervous system, it can help them overcome some cognitive and physical effects. However, at least 40% of those suffering from insomnia long-term report experiencing some symptoms.
Insomnias And Depression: Anxiety And Depression.
Anxiety and psychiatric disorders are a leading cause of insomnia symptoms.The inability to sleep is a common sign of many mood disturbancesThis includes:
- Depression. Difficulty sleeping may be one of the first symptoms of depression. In fact, there is evidence to suggest that acute insomnia is frequently related to the first onset of depression symptoms
- Schizophrenia
- Social phobia
- There are two phases to bipolar disorder: the manic and depressive. Manic episodes can be triggered by lack of sleep due jetlag or other causes.
- Post-traumatic stress disorder. Disrupted sleep and nightmares are common symptoms of post-traumatic stress disorder. Paranoia, fear, hypervigilance and paranoia can make sleeping difficult or impossible. Insomnia may be caused by flashbacks, as well as hallucinations and talking or shouting during sleep. Patients with PTSD may be awakened from their sleep by movements like punching or kicking.
Insomnia can also be caused by medications that treat psychiatric disorders.. Psychotropic medication may cause sleep disruption by their stimulating effects. Antidepressants, other medications used to treat mood disorders, may trigger or exacerbate restless leg syndrome or periodic limb movements.
Which Came First, The Mood Disorder Or The Insomnia Symptoms?
Once, it was believed that insomnia symptoms were caused by psychiatric disorders or depression. Now the evidence isnt so clear.Not only are sleep problems caused by emotional disturbances but they can also increase the risk of suffering..
An analysis of major studies revealed that study subjects who suffered from insomnia symptoms were twice as likely to be diagnosed with depression as those without sleep difficulties.
Why? Though the connection between mood disorders and insomnia isnt entirely clear, it is well-known thatSleep disturbances can affect hormones and neurotransmitters.. Sleep is a restorative activity that helps reduce stress levels in the body. Excess secretion of cortisol – also known as the stress hormone – may play a role, as well.
People with insomnia symptoms may be more likely to experience physiological stress and lack of sleep. It is important to seek treatment for chronic insomnia and other sleep disorders as soon as possible, especially if there are any family histories of psychiatric disorders.
Insomnia Facts: Many insomniacs have somniphobia, a fear of sleeping. Symptoms typically include extreme dread of going to sleep, as well as anxiety, feelings of panic, and shortness of breath
The Insomnia Myths Vs. Reality
Myth: Insomnia Only Happens To Anxious People
Reality: Insomnia symptoms can happen for a vast number of reasons. Although anxiety is a common cause of insomnia, it’s only one factor that can trigger this condition.
Myth: Insomnia can be defined as the inability to fall asleep.
Reality: Insomnia might involve the inability to fall asleep, or manifest as frequently waking during the night, waking early, or feeling sleepy during the day. Someone who can fall asleep quickly may still be diagnosed with insomnia if they cant remain asleep, wake too early, or suffer from fragmented, low-quality sleep.
Myth: If You Cant Fall Asleep, You Should Lie In Bed Until You Do
Reality: Remaining in bed when you cant sleep may signal to your brain that your sleeping environment is where you lie awake. This can also increase anxiety and make it more difficult to fall asleep again. Most experts agree that if you dont fall back to sleep within 15 or 20 minutes of waking up, its best to get out of bed and participate in a relaxing activity such as listening to soothing music or reading.
Myth: Alcohol and television can help combat insomnia symptoms
Realism: It has been shown that alcohol can impair sleep quality, and increase the likelihood of waking up during the night. Television, especially the news, can make relaxation difficult and stressful. Additionally, TVs, smartphones, and computers emit the blue light well-known for interfering with sleep-wake cycles.
Myth: It Doesn’t Matter If You Wake Up For Short Periods Of Time During The Night. This Won’t Affect Your Quality Of Sleep.
Reality: While a brief interruption to your sleep may seem insignificant, waking up during the night for more than a few minutes can result in a loss of sleep. Studies show that interrupted sleep can be just as harmful as inadequate sleep.
Insomnia Fact: On average, parents lose 44 days of sleep within the first year following the birth of a baby
How To Cure Insomnia
The cure for insomnia may not be as simple as taking a pill or counting sheep, buteffective treatments do exist. There are many remedies for insomnia symptoms that differ from those for sleep disorder.The following are possible treatments for short-term or mild insomnia symptoms:
- For those suffering from insomnia caused by a medical condition, address the underlying cause. For example, if trouble sleeping is partly the result of asthma symptoms, a more effective asthma treatment plan may reduce or eliminate insomnia
- Lifestyle changes. Exercising regularly, eating well, avoiding alcohol and stimulants, eliminating nicotine, and creating a relaxing bedtime routine can all help promote high-quality sleep
- Sunlight exposure
Getting plenty of exposure to daylight, especially in the morning, helps maintain the bodys natural circadian rhythms, which are responsible for maintaining a consistent sleep-wake schedule
How To Stop Chronic Insomnia
Though it may contradict much of what weve heard about treating insomnia, good sleep hygiene is often not an effective treatment for chronic insomnia.
While good sleep hygiene can reduce persistent insomnia problems, it is not the first-line treatment.
What is help? Paradoxically,one of the most effective chronic insomnia treatments is reducing the number of hours spent in bed. This type of treatment isPart of the Cognitive Behavior Therapy protocolFor chronic insomnia This protocol includes:
1.Restriction on sleeping. Sleep restriction requires limiting the time spent in bed to the number of hours typically spent asleep.For example, if you usually spend eight hours in bed but lie awake for two, sleep restriction therapy might require you to go to bed at midnight and get up at 6 am. This type of treatment is more beneficial than going to bed earlier.
Though it may seem to compound the problem of insomnia, sleep restriction therapy increases sleep efficiency and cuts down on waking during the night. Training a person to sleep well for at least six hours without awakening may allow them to add 15-minute blocks of time to their bedtime, gradually increasing until they feel rested throughout the day.
2.Training in stimulation control.This will help chronic insomnia sufferers to reduce negative associations with their bedroom environment and sleep. Training essentials include:
- Lying down in bed only when sleepy
- Using the bed only for sleep and sex
- If you are unable to fall asleep after 20 minutes, get up and go back to bed when you feel sleepy. Repeat if necessary
- Getting up at the same time every morning
- Foregoing naps
This type of therapy protocol can train the brain to associate a particular environment and time of night with sleepBreak the cycle of sleep disorder that results in poor quality, delayed or fragmented sleep.
3.Relaxation training. This type of training teaches insomnia sufferers to use a combination of meditation techniques, guided imagery, and breathing exercises to prepare the body for sleep.
Biofeedback helps patients learn to control the bodys normally involuntary bodily processes, such as heart rate, blood pressure, and muscle tension.
Combining these techniques can help you relax your body and calm your mind so that it is easier to fall asleep.
4.Psychotherapy. This aspect of the protocol involves challenging negative beliefs about sleep, and replacing fearful associations with positive thinking. The evening and before bed can be used to relax, so worry may be reduced to a specific time of the day. Insomnia patients in cognitive behavior therapy learn to manage stress and control the over-active thought process that may lead to sleep difficulties.
Sleep Hygiene – A Good Start For Mild Insomnia
Although it is not recommended for chronic insomnia, good sleep hygiene can help with milder and more persistent symptoms.
These are some of the best sleep hygiene tips:
- A regular sleep-wake routine
- Using the bed only for sleep and sex
- Avoiding the blue light exposure from electronics and smart phones in the hours leading up to bed
- Ensuring that your bedroom stays cool, dark, and quiet
- Make sure you invest in comfortable bedding and a mattress.
Although insomnia is common, it does not have to be a chronic condition.. It is possible to get back to restorative sleep by addressing the problem quickly, treating the underlying conditions and practicing healthy sleep-promoting habits.
References
- Swapna Bhhaskar, Prevalence and Correlation of Chronic Insomnia among Adult Patients and Medical Comorbidities. Journal of Family Medicine and Primary Care,Oct.2016
- Paula Alhola. Sleep Deprivation and Cognitive Performance. October 3, 2007. Neuropsychiatric Diseases and Treatment
- Bonnet MH and Arand DL. Hyperarousal and Insomnia: State of the Science. PubMed NCBIFeb. 14, 2010
- Rachel E. Salas, Increased Use-Dependent Plasticity in Chronic Insomnia. March 1, 2014,PubMed Central
- Mahesh M. Thakkar, Alcohol Disrupts Sleep Homeostasis, June 1, 21015,PubMed Central
- Sleep Patterns and Insomnia Among Adolescents: a Population-Based Study, Mari Hysing and Stale Pallesen, Marc 8, 2013, European Sleep Research Society
- Sharon Schutte-Rodin, M.D.
Lauren Broch, Ph.D. Clinical Guideline for Adults with Chronic Insomnia
Journal of Clinical Sleep Medicine Research & Review Articles In Sleep Medicine, July 2008